Eleanor Turnbull-Jones is an Infectious Diseases/General Medicine doctor in training at Cambridge University Hospitals NHS Foundation Trust (CUH) and a Global Health Fellow. Here she explains why she took on the fellowship and the impact she’s been able to have working within the Kampala-Cambridge Health Partnership.
“I have worked in global health projects for nearly twenty years, since starting up my own NGO to improve the health and education of children in 2005. I have worked in India, Sri Lanka, Rwanda, Zambia and Nigeria and Kenya on a variety of health projects and clinical research trials.
I was keen to continue my involvement in global health projects while being based in Cambridge for my Infectious Diseases training, and the Global Health Fellowship scheme was the perfect opportunity to do this.
I’m involved in the CwPAMS project within the Kampala-Cambridge Health Partnership, which aims to improve maternal and neonatal health by addressing antimicrobial resistance (AMR) specifically. Infection prevention & control (IPC) and antimicrobial stewardship (AMS) are targeted as areas for development at Kawempe National Referral Hospital (KNRH). This is a project that has been ongoing for numerous years and there are good relationships between the partners, enabling honest and frank conversations about interventions that would be beneficial.
It was very rewarding to meet the clinical staff from the hospital who were all so committed to improving patient care. They were surrounded by significant logistical challenges but remained upbeat and optimistic about their work.

My contribution
I visited Kampala in October 2024, during the CwPAMS 2 phase of the project, with the goal of meeting the Kampala partners to determine the activities completed since the last visit and throughout the entire grant period to write the end of grant report.
Alongside this, the project aims to strengthen and expand the AMS work at KNRH, now the hub site. Results from previous visits and from the continued work carried out by local partners, have shown that most of the antimicrobial use remains empirical. An important next step to expand the AMS project relies on the development of local microbiological laboratory testing facilities to allow identification of resistance patterns in infection and promote targeted antimicrobial treatment.
I was involved in several key tasks during the visit:
1) I interviewed key staff in the hospital to understand the challenges and review the successes of AMS interventions that have been put in place, such as surveys (GPPS) of antimicrobial use in the postnatal ward and NICU.
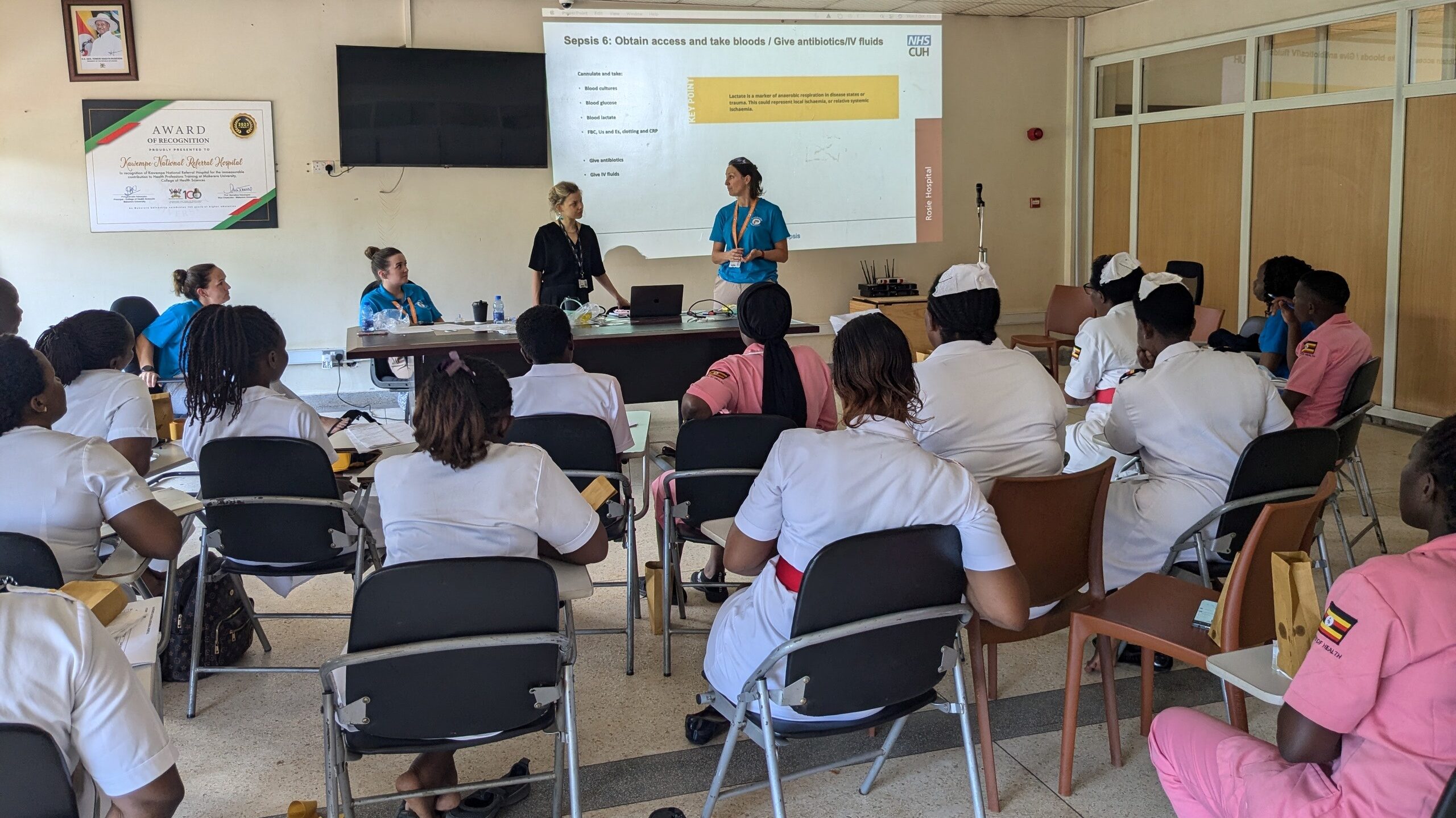
2) I supported the teaching of relevant clinical staff on identifying sepsis and the importance of taking microbiology samples from these patients and sending to the lab for processing.
3) I helped to conduct a pilot study to assess the feasibility and acceptability of doing a community prevalence study in pregnant women attending the antenatal clinic at KNRH to review ESBL/MRSA colonisation. The results of this pilot study will be used to apply for ethics approval and will allow the hospital director to ensure that empirical antibiotic guidelines in the hospital are appropriate for the community.
Reflecting on the experience
My previous experience living and working in Eastern and Southern Africa meant I adjusted very quickly when I arrived. Having managed projects and research trials in local health clinics in Zambia also meant I could quickly organise how to set up the pilot study in the antenatal clinic and efficiently conduct this with my colleagues.
It was challenging to be in the country for such a short period of time as it felt that we had only just arrived when we had to leave. I can see there is a great need to improve the laboratory in the hospital and it was frustrating not to be able to fix this. Working in partnership with a hospital is difficult because you do not have the authority or responsibility to implement new guidelines and the role instead is more of a mentoring role which can takes longer to develop but is understandably more meaningful and sustainable in the long run.
It was very rewarding to meet the clinical staff from the hospital who were all so committed to improving patient care. They were surrounded by significant logistical challenges but remained upbeat and optimistic about their work.
This experience has reminded me of my love for being in Africa and it was wonderful to go back after so many years. It has reminded me that the NHS is incredibly lucky to have the resources and trained staff that we have and given me more awareness for how privileged we are to have our health system.
Professionally, the experience gave me the opportunity to plate and identify bacteria with the supervision of a senior microbiology registrar which is an excellent introduction to microbiology before my training in this speciality starts in the next year.


Impact of the visit
We trained around 30 members of staff on recognising and treating sepsis and the importance of taking blood cultures so I hope that this will have an ongoing impact for improving patient care in the hospital.
We worked with the antenatal clinic staff to do our pilot study to review community ESBL and MRSA rates and have fed this back to the hospital and the midwives so they are aware of the high rate of resistance to ceftriaxone in the community. We hope that this will allow the hospital to develop their guidelines for empiric antibiotic treatments.
We worked with the laboratory staff to discuss the importance of processing more samples from patients and sending to the reference laboratory for further identification. I hope that this will enable better microbiology identification and thus improve patient care with more targeted antibiotic therapy.
Back home, the visit has made me more aware of microbiology sensitivities and the impact of community-acquired MRSA and ESBL which I need to be aware of when prescribing in the hospital.”
I would recommend global health work to everyone. I think it gives a greater outlook and enables us to understand the importance of global health. It benefits our mental health because despite sometimes feeling frustrated working in the NHS, once you have seen other healthcare systems you return feeling prouder of the NHS and what it can achieve

Find out more about the Working to improve maternal and neonatal health project, or contact us at info@cghp.org.uk
Return to blogs

