Pre-deployment training for NHS resident doctors preparing to work in a low resource country took place in Cambridge last week. Organised by Cambridge Global Health Partnerships (CGHP) in collaboration with NHS England’s Global Health Volunteer Programme, the intensive three-day course provides practical guidance, skills and advice to enable resident doctors to work safely, effectively and ethically in clinical settings outside the UK.

Inspiring (and managing) expectations
Day one provided the inspiration for getting involved in global health, as well as emphasising the importance of taking an open-minded and humble approach. “Ego is what kills patients,” explained paediatric emergency doctor Jo Langton. “Working internationally isn’t about you. You’re keeping the seat warm until the next person comes along. You’re helping the people you leave behind become better at what they do,” she added.
The importance of listening, adapting and being culturally aware was a sentiment echoed by many of the presenters, who advised that global health is something you can prepare for but never truly be ready for. The speakers emphasised the huge amount of skill and knowledge gained through exposure to practical, hands-on work, but also shared strategies for self-care to cope with often overwhelming situations and need.
The evening dinner that night was filled with the buzz of excited and inspired conversation, as delegates were able to connect with Global Health Volunteer Programme alumni and delve deeper into their experiences.


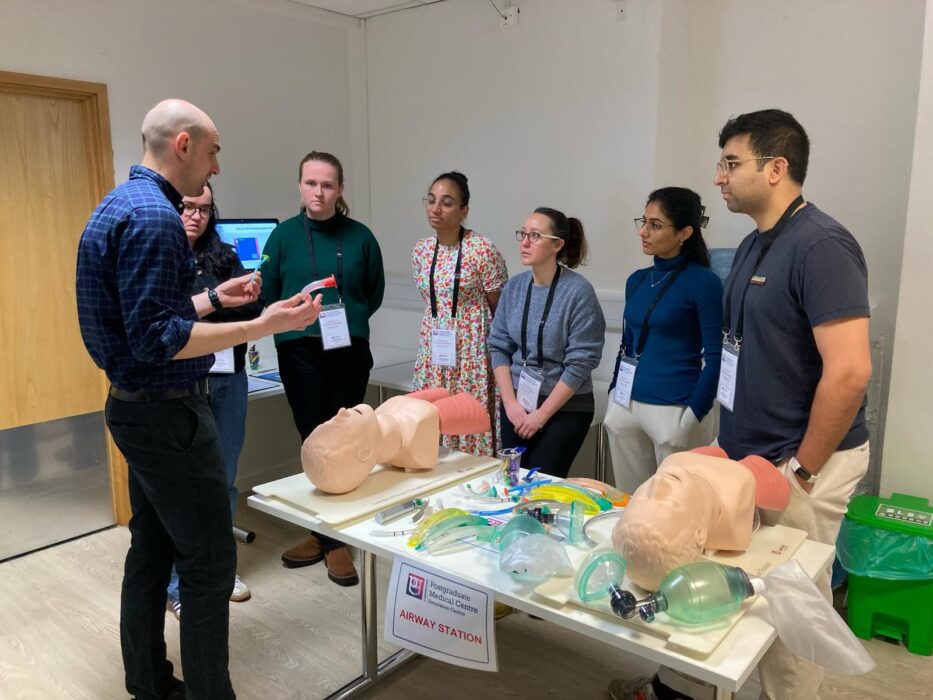
Hands-on skill training
On day two, participants had the opportunity to customise their learning experience by focusing on paediatrics, obstetrics or adult medicine, allowing them to choose areas most relevant to their interests and placements. The sessions provided hands-on training that enabled the resident doctors to develop technical skills and practice basic medical procedures using models to simulate real-world conditions.
Day two also covered important topics like snakes and snakebites, a constant hazard in rural Africa, equipping participants with the knowledge to handle these types of medical emergencies.
Day three provided even more hands-on training, including sessions on orthopaedic scenarios, chest drains and identification and management of HIV and TB.
It included an important session focused on defining ethical considerations and exploring the role ethics plays when undertaking placements in resource-limited settings. Conducted as a group discussion, the residents were able to share their perspectives on what ethics means to them and identify potential ethical dilemmas they might encounter while working internationally.
The thought-provoking conversation considered how ethical standards might vary between their home country and the host country, emphasising the importance of cultural sensitivity and adaptability.

Key takeaways
Over the three days, the key theme that emerged was the complexity and subjectivity of ethics in global health. Participants acknowledged that:
- Ethical dilemmas are often situational and may not always have clear-cut answers.
- Cultural context plays a crucial role in ethical decision-making, requiring adaptability and open-mindedness.
- Balancing personal and professional ethics with local healthcare norms can be challenging but is essential for building trust and delivering effective care.
- Collaboration with local colleagues and communities is key to navigating ethical challenges and ensuring respectful and sustainable healthcare practices.
Finishing the workshop with the opportunity to discuss and reflect on these ethical responsibilities and develop a framework for making informed decisions was very valuable. It will help ensure this group of resident doctors go into their placements with the skills, knowledge and confidence to ensure their contribution to global health is safe, effective and ethical.
Find out more about NHS England’s Global Health Volunteer Programme.
If you’re based in the East of England, you could apply for CGHP’s Global Health Fellowship scheme. It’s open to doctors in training (ST3 and above in all specialties), Nurses and Midwives doing their preceptorship, and AHPs in their final year of training.
Return to news

