By Chiara Valentini
Chiara Valentini is a CGHP Global Health Fellow and a Registered Midwife at the Rosie Hospital. Here she explains the personal and professional growth and learning gained from just one week working alongside Ugandan healthcare staff.
“I have always been passionate about health inequalities and global maternal and newborn health. I trained in Italy, work in the UK and completed a MSc in Global Maternal Health through which I had the opportunity to complete a placement in an NGO in Indonesia. Since then, my interest in global health matured exponentially out of the desire to have a meaningful impact on maternal and neonatal outcomes and contribute to stronger, more sustainable health systems through collaborative partnerships where each side gets opportunities to grow.
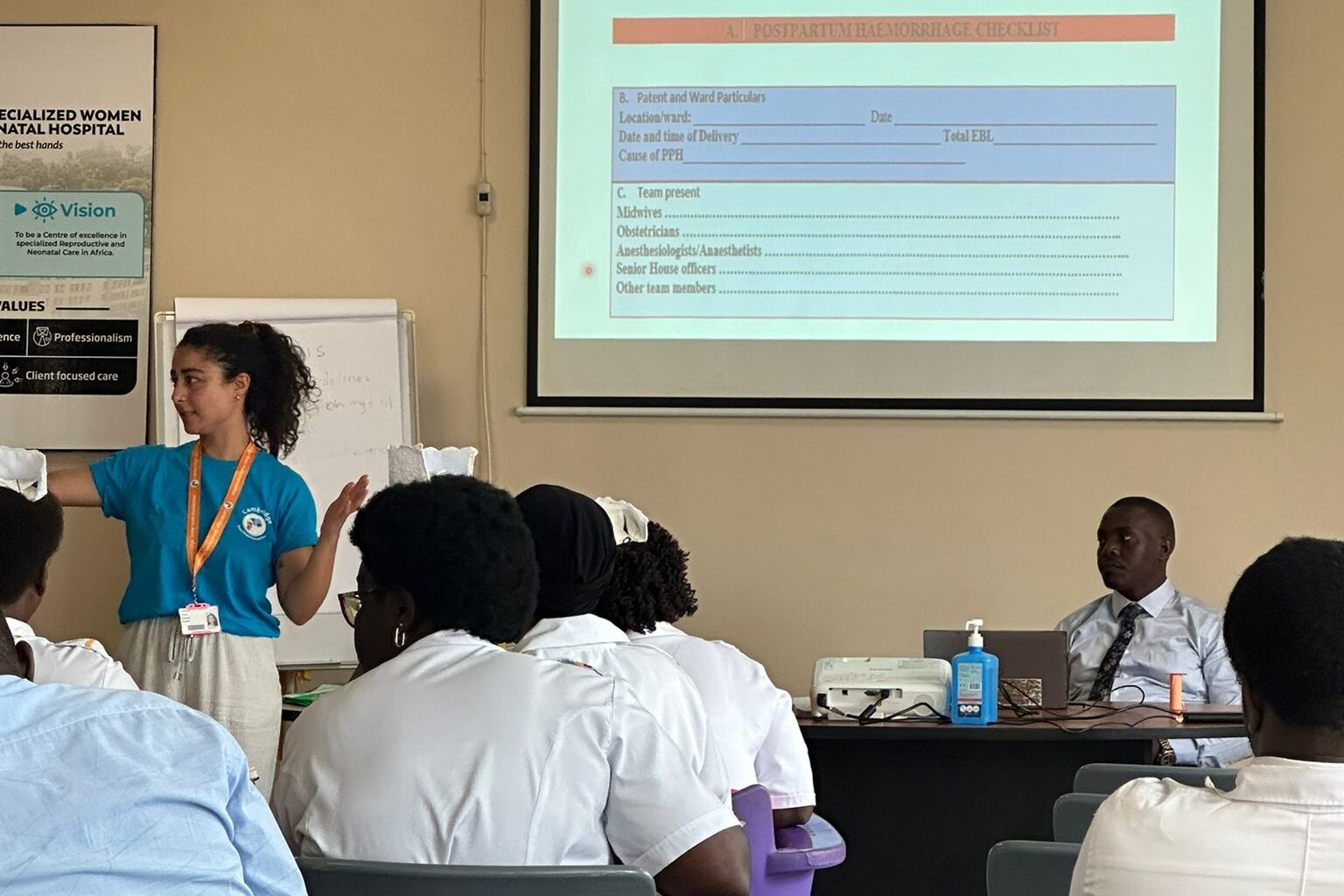
Through my Fellowship, I’m involved in the Maternal and Neonatal Health Guidelines project – part of the Kampala-Cambridge Health Partnership. In collaboration with Ugandan healthcare professionals, the project is developing context-specific maternal and neonatal guidelines on obstetric emergencies using evidence-based recommendations. The aim is to strengthen clinical practice and improve early diagnosis and emergency response to improve health outcomes for women and newborns in Uganda.


Fostering sustainable change
A crucial part of this project has been long-term collaboration between institutions in the UK and Uganda, and to create a sustainable train-the-trainer model for the Ugandan team to continue to thrive and lead transformation within their local context. Rather than a top-down approach, the work is collaborative, grounded in respect for local expertise, and aimed at producing guidelines that are both clinically robust and practically implementable. Throughout my Fellowship year, the UK and Ugandan teams have co-produced guidelines based on the pre-existing National Ugandan Guidelines and tailored them to Kawempe National Referral Hospital and Mulago Specialised Women and Neonatal Hospital in Kampala. The opportunity to engage throughout the year virtually, and then to meet in-person in the UK and in Uganda, created a powerful space for shared learning and exchange.

Sharing knowledge and skills from a midwifery perspective
I participated in the train-the-trainer process to support the local staff to develop their teaching skills, delivering a presentation on the topic of ‘communication’, helping new trainers give presentations, and facilitating simulation stations and debriefing sessions. I shared UK best practices around obstetric emergencies and evidence-based practices, team debriefing and communication with patients, while learning from Ugandan colleagues about the challenges and strengths of the local health system.
My contribution centred on supporting and delivering PRactical Obstetric Multi-Professional Training or ‘PROMPT’. In doing so, I was able to offer a midwife’s perspective on emergency responses, support multi-disciplinary team debriefing, promote evidence-based practice, and advocate for the inclusion of respectful care principles. The team appreciated my midwifery support in facilitating conversations and debriefings around how to make guidelines practical and woman-centred.
It was incredibly refreshing to connect with people working in another country who share the same values and passions, even while navigating very different challenges. It reminded me that—despite varying guidelines, systems, and levels of privilege—we are all working toward the same goal: improving care for women and newborns. That sense of shared purpose is powerful.

Challenges and rewards
It was difficult to reconcile ideal, evidence-based recommendations with the realities of limited resources, structural and systemic barriers. Finding the balance between the gold standards of my own setting and what was feasible locally required adaptability, cultural sensitivity, and above all, a willingness to be guided by the Ugandan team’s insights and experience.
The most rewarding part was witnessing the incredible commitment and resilience of Ugandan healthcare professionals. Their eagerness to engage in meaningful dialogue during team debriefs and to learn from each other’s experiences was truly inspiring. The spirit of collaboration and mutual respect reminded me of the power of collective effort in global health.
The visit has broadened my worldview, deepened my appreciation for cultural diversity and the value of stepping outside our comfort zones. It was incredibly refreshing to connect with people working in another country who share the same values and passions, even while navigating very different challenges. It reminded me that—despite varying guidelines, systems, and levels of privilege—we are all working toward the same goal: improving care for women and newborns. That sense of shared purpose is powerful.
Professionally, this experience has strengthened my confidence in teaching and facilitation—whether through simulation, team debriefs or lectures. It reinforced how essential it is to nurture a culture of care within teams, where we learn and grow together to improve outcomes. It also made me more reflective about my own practice and reinforced the importance of cultural humility, listening actively, and creating space for others’ voices. These are skills I’ll carry forward in every professional setting.

Trusting in the process
One of my favourite moments happened on the very first day. The training was running over three hours behind schedule, and—still very much grounded in UK-style timekeeping—I couldn’t help but worry: “Will we finish on time?” “Will we manage to cover everything on the agenda?” By the time the morning session wrapped up (well into the afternoon!), the Ugandan team was getting ready for the lunch break. Meanwhile, I was still caught up in my thoughts and worries and immediately started prepping for the simulation sessions—setting up equipment, organising the rooms, asking questions about timings and logistics. To my surprise, everyone looked at us with a bit of confusion and reminded us to rest and enjoy the food.
That moment really stayed with me. I loved how calm, grounded, and adaptable the Ugandan team was—shaping the day around the people, not the schedule. It was a powerful reminder to slow down, be present, and trust the process.
Measuring the impact
The visit will support practical improvements such as reducing delays in emergency care, improving communication and strengthening teamwork. It will also promote sustainable training methods that build the healthcare staff’s confidence and capacity—led by and grounded in the local context, rather than driven solely by external input from the Cambridge team.
I have returned to the UK witha deeper understanding of guideline development and implementation, particularly in resource-limited settings, including effective train-the-trainer approaches.
For example, at Kawempe Hospital I saw how a simple bucket serves multiple practical purposes—used as a container for personal belongings, a birthing stool and a washing basket. This simple, low-cost tool supports labour progress and infection control by keeping personal items contained and off the bedspace. In high-resource settings like the UK, we can sometimes overlook these inventive, simple solutions. This experience has reminded me of the value of practicality and adaptation—sometimes the simplest tools can make a big difference in patient care.

Final reflections
Global health work is a powerful way to get the excitement back, often lost in our daily work life. I believe every healthcare professional would benefit from seeing how others work and from contributing to efforts that go beyond our local context. Partnerships such as the one I have the honour to be part of, are precious to ensure sustainable improvement and connections.
I would love to stay involved in global health, ideally through CGHP. I am keen to continue doing my part and contribute to reducing maternal and newborn morbidity and mortality. I have built a strong connections with Ugandan midwives and I am sure we will find opportunities to continue this partnership and share learnings!”
Find out more about the Guidelines Project or contact us at info@cghp.org.uk
Return to blogs

