Mercy Rebecca Adera is a staff nurse at the Rosie Hospital. Originally from Kenya, here she describes the experience of helping to deliver training in infection prevention control, management of sepsis and obstetric emergencies in Kakamega, western Kenya.
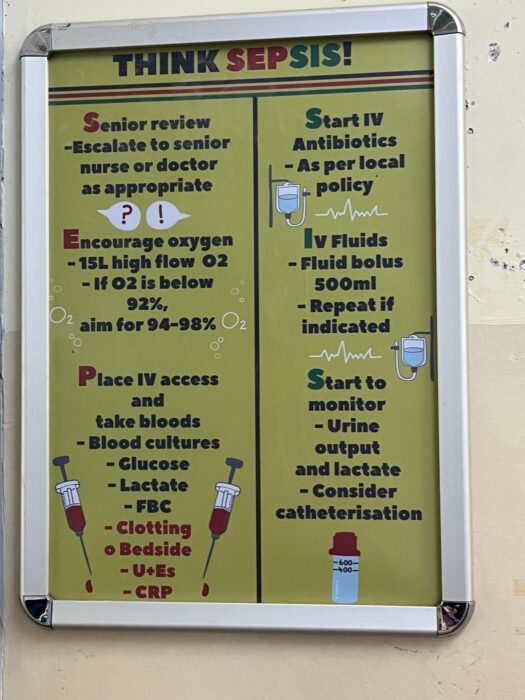
Mercy Rebecca Adera is a staff nurse at the Rosie Hospital, part of Cambridge University Hospitals Trust. Originally from Kenya, in March she joined a team from Cambridge visiting the Kakamega-Cambridge Antimicrobial Stewardship partnership to help deliver training with local faculty at Kakamega County General Teaching and Referral Hospital (KCTRH) on infection prevention control, management of sepsis and obstetric emergencies.
The visit was also a chance to recruit and train local champions at KCTRH to enable them to continue delivering a similar course at KCTRH and across the region. This ‘train the trainer’ approach, as well as the setting up of quality improvement projects, is about making sure practice change is lasting and sustainable.
Here Mercy tells us more about the visit and why she is motivated to work in global health.

What inspired you to get involved in global health?
“The desire to share knowledge with the health workers back in my country of origin in order to create better healthcare outcomes for the patients.”
What is unique about the Kakamega-Cambridge Antimicrobial Stewardship partnership?
“It involves sharing of knowledge and coming up with strategies between the Kakamega and Cambridge team to best practise infection prevention and control and to address the major causes of maternal mortality in order to prevent maternal morbidity and mortality.”
What were your key tasks and responsibilities during the visit?
“I flew to Kenya a week earlier than the rest of the team so that I could organise the team in Kakamega. I ensured the learning hall was booked so that we had an area to conduct the training. I ensured the medical superintendent was aware of our visit and booked a time slot to visit her office and introduce ourselves. We came up with a programme on how the trainings would be conducted and booked slots for meetings with the Ministry of Health and with Masinde Muliro University.”
What expertise did you contribute and where did you make the biggest impact?
“I had the knowledge and experience of how the Kenyan health system conducts their activities. I was able to bridge the gap between the Kenyan team and the Cambridge team having previously worked in Kenya and now in Cambridge.”

What did you find the most challenging and the most rewarding parts of the experience?
“The most challenging part was organising the training as we had hoped to include doctors in our training, but they were on strike. Doctors can prescribe medications and rule out maternal obstetric emergencies thus were an important pillar. Nevertheless, the enthusiasm among the nurses gave me hope that they also had acquired the necessary knowledge required to manage the maternal obstetric emergencies and perform infection prevention and control. I was also happy that quality improvement projects were identified as this will enable the sustainability of the trainings and knowledge taught during the week. The presence of hand hygiene posters all over the hospital that we created the previous year were an indicator that the staff remembered the infection prevention process and were practising them. The establishment of a hand gel production unit also helped with regards to hand hygiene.”
How has the experience developed you personally?
“I have become a more assertive individual because during the visit we had to make decisions regarding the training and stick to our agenda. The doctors’ strike taught me to appreciate that we cannot control everything and we should work within our means to achieve the best.”
How has the experience developed you professionally?
“I have been able to deliver theatre induction training to the newly recruited midwives in my department. I found it easy to prepare and present because of the confidence and communication skills that I acquired while delivering the teaching at Kakamega and interacting with staff from different specialities.”
Please describe your favourite anecdote or experience of the trip.
“My favourite experience was going back to reflect on the training we had delivered in the previous two years. Some of the staff recognised what we had taught so that was an indicator that some impact was made.”
What impact will the visit have on healthcare staff and patients in Kenya?
“The healthcare staff have reinforced knowledge on maternal emergencies and infection prevention and control. The patients will now have better health outcomes because the staff are able to manage their conditions and respond promptly to them.”
Would you recommend global health work to your colleagues and if so, why?
“Yes because it gives us a chance to give back to the communities in lower income countries and have a positive impact on the healthcare systems.”

Find out more about the Kakamega-Cambridge Antimicrobial Stewardship partnership. If you are interested in supporting CGHP, please follow the donate button below or contact the team.
Return to blogs

