By Lisa Enoch
Lisa Enoch is Critical Care Education Lead at Cambridge University Hospitals NHS Foundation Trust (CUH) and co-lead of the SCALE Critical Care project between Cambridge and Kampala. Here she explains the impact of a week of face-to-face learning in embedding skills and knowledge for both UK and Ugandan nurses.
“Spending a week in Kampala, Uganda, alongside four passionate nurses, a resuscitation officer and a midwife was a privilege and a profound reminder of why global health partnerships matter. Working across two sites, we collaborated with local teams at Mulago National Referral Hospital to deliver “Train the Trainer” workshops focused on teaching skills and simulation-based education for critical care nurses.
In-person visits are an important component of health partnerships but this one was different. It wasn’t just about delivering training: it was about the true essence of building capacity and creating sustainability. We have long since recognised our colleagues in Uganda have vast critical care knowledge and very adaptable skills. Our aim was to equip senior nurses with the ability to confidently design teaching sessions with clear learning outcomes, deliver structured presentations, and lead simulation sessions with a meaningful debrief. By doing so, we are not just sharing knowledge but investing in unit leaders who can continue to drive education forward long after we return to the UK.


Bidirectional learning: a two-way street
As always with our time in Uganda, the learning was bi-directional. Our nurses came away inspired, having honed their own teaching, communication and leadership skills in a challenging yet deeply rewarding environment. The resilience, adaptability and clinical ingenuity they witnessed in the Ugandan nurses will undoubtedly inform and enhance their practice back in the NHS.
These are the kinds of experiences that shape reflective practitioners and future leaders – this was already evident in our conversations in the evenings. We all agree there is much to learn in being more generalist in our approach to critical care delivery: our Ugandan colleagues can look after any age and complexity from maternal patients to child trauma to adult cardiac all on one unit. We have become very specialised in the UK and this has reduced our resilience and flexibility within our workforce and created silo working.

Addressing the structural challenges
Yet, amid the success, one concern remains personal and persistent for me: nursing establishments remain a challenge and nurse-to-patient ratios are not yet standardised within critical care. Our Ugandan colleagues have told us how critical care nursing still isn’t recognised as a priority in the healthcare system, which I believe is rooted in the lack of robust outcome data. But the nurses know and they feel the difference their care makes in patients’ recovery and outcomes. The stories they shared spoke volumes.
With that in mind, we decided with the senior Ugandan nurses to carry out an evaluation of resuscitation and cardiac arrest to highlight several elements:
- the enhanced skills CC nurses have
- the response and outcomes to the defibrillator and good basic life support
- the response time needed for a positive outcome (and therefore enough staff on the unit for each shift)
CUH Critical Care Nurse Ellie Walsh is working with lead consultant Dr Jane Nakibuuka in Kampala to design the audit form for this piece of work.
In-person visits are an important component of health partnerships but this one was different. It wasn’t just about delivering training: it was about the true essence of building capacity and creating sustainability….By doing so, we are not just sharing knowledge but investing in unit leaders who can continue to drive education forward long after we return to the UK.
Raising the profile of critical care nursing
One of the most impactful moments of the week for me was meeting with the Head of the Ugandan Critical Care Nursing Association. We discussed piloting a new ICU competency framework that could act as a passport of skills, competence, and knowledge for ICU nurses nationwide.
This initiative, if endorsed by the Ugandan Nursing Council, could transform how critical care nursing is viewed, structured and developed across the country. It’s an ambitious project, but one with deeply meaningful potential. It formalises what we already know: these nurses are highly skilled professionals delivering complex care.
Last year Ugandan nurse Sr Martha Alupo and CUH Critical Care Nurse Livi Reese established a ventilator care bundle audit, which they are incredibly proud of. On this visit, we had the opportunity to really examine the data, and it is amazing. The nurse in charge had created a wonderful spreadsheet. We discussed how we will now provide support to publish this with Ugandan staff being the lead authors – contributing to nurse-led research and publications, and raising their profile.
Sustainable change through mentorship
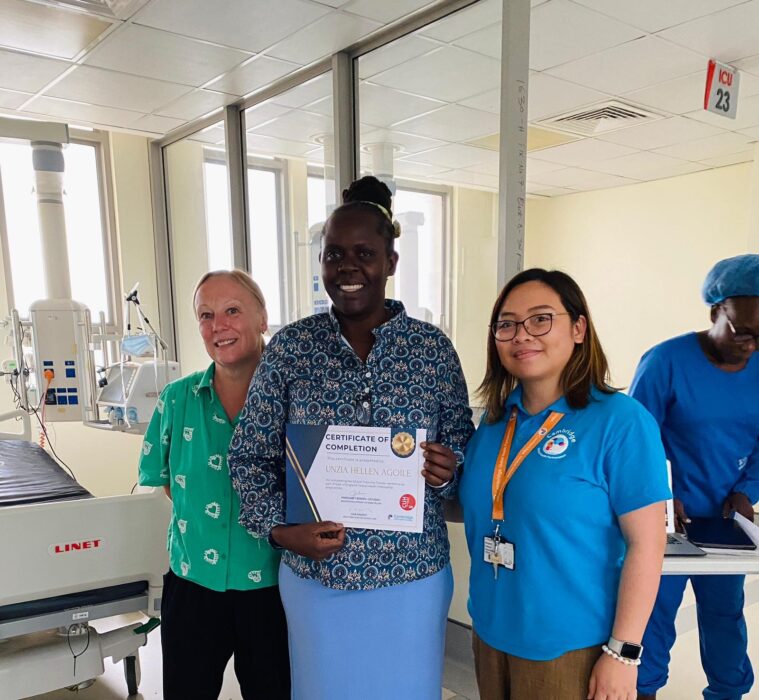
We’ve now trained eight exceptional Ugandan nurses to become local educators. They will carry this work forward, mentoring peers and fostering the competency framework’s rollout. Our UK team will remain connected, offering remote support where needed, ensuring that the work continues in collaboration—not imposition.
This work is not just about training—it’s about solidarity, shared growth and raising the global profile of nursing. It reminds us that excellence in care is a universal goal and that we are stronger when we learn from one another. By investing in teaching, by empowering local leadership, and by advocating for systems that value critical care nursing, we are taking meaningful steps toward global health equity.
Final reflections
Our time in Kampala was filled with challenge, collaboration and immense learning. It reminded me that transformation in healthcare doesn’t always come from grand gestures, but often from small, intentional acts: a nurse learning how to deliver a simulation or a conversation that sparks systemic change. I was super proud of the team; they worked hard and were very humble.
We left Uganda with full hearts, renewed purpose and a shared vision—that through partnership, nursing can lead change, both at home and across the globe.”


Find out more about the SCALE Critical Care Project or contact us at info@cghp.org.uk
Return to blogs

