By Jennifer Wilburn
In this blog, Global Health Fellow Jennifer Wilburn details her experience with the Antimicrobial Stewardship and Infection Prevention Control (IPC) project in Kampala, Uganda, helping to better understand antimicrobial resistance (AMR) and antimicrobial stewardship (AMS) knowledge and practices among individuals who dispense antimicrobials in community settings.
Jennifer Wilburn is a 2023 East of England Global Health Fellow and formerly a Public Health specialist trainee. She is currently completing a Postgraduate Certificate from the University of Cumbria on Humanitarian Action and Disaster Response as part of her Fellowship. Jennifer has a long-standing interest in global health and infectious diseases.

Background
On 03 June 2023 I boarded a plane to Kampala, Uganda for a two-week trip to undertake data collection for my Global Health Fellowship project. My journey to get to this point has been a long one. I’ve always been interested in global health; I’m fascinated by infectious diseases and how human interactions and global movements contribute to their spread, so I have tailored my experiences to learn more about this. I received my master’s degree in Global Disease Epidemiology and Control back in 2012 and spent two months in Burkina Faso, West Africa, working on a research project focusing on understanding HIV risk factors among most at-risk populations. During that time, I worked with colleagues from the Ministry of Health, attended focus groups with individuals from the target populations, travelled to the countryside to sit on a crocodile (not joking), and danced at a local wedding. It was an amazing experience and I resolved to return to the African continent one day.
I joined the public health training programme in 2019 with the aim of becoming a Consultant in Global Public Health. I was assigned to the East of England and quickly became aware of the lack of global health placements for public health trainees. There were ample opportunities for medical trainees from other disciplines, but strangely not public health.
Then, in 2020 I received an email from our Head of School that changed everything. She was asking for a volunteer to work with CGHP to set up a Global Health Fellowship for different disciplines, including public health! I jumped at the chance and, over the next few months, I worked with CGHP Director Evelyn Brealey and others to shape a Fellowship that would benefit not just the trainees, but CGHP and its partners as well. The first call for Fellowships went out in Spring 2021 but unfortunately I did not meet the ST level required to apply. However, in 2022 I applied and was offered one of two Fellowship positions for Public Health Trainees.
The partnership project
One of the things that attracted me to the Fellowship in the first place was the opportunity to work closely with in-country partners on issues that were important to them. And, of course, the potential opportunity for an overseas visit. After hearing about the different projects that were already ongoing, I was intrigued by the Antimicrobial Stewardship and Infection Prevention Control (IPC) project in Kampala, Uganda. Colleagues from CGHP, Makerere University in Kampala and the Infectious Disease Institute (IDI) in Kampala were planning to undertake a project to better understand antimicrobial resistance (AMR) and antimicrobial stewardship (AMS) knowledge and practices among individuals who dispense antimicrobials in community settings in Kawempe Division, Kampala. This project was borne out of the realisation that CGHP and partners were engaging in a lot of work within a hospital in Kampala to promote AMS, but anecdotal evidence was showing that many patients actually visited community dispensary settings to obtain their prescriptions. There was little published evidence on knowledge or practices in these settings. I could really see how the findings from a study like this would be extremely beneficial to the local population and policy makers, so I joined the team.
From September 2022 to the end of May 2023, the majority of my time went into meeting with partners, co-developing the protocol and associated documents, submitting them for ethical approval and planning for data collection. Finally, after five months we had all of the approvals and it was all systems go.

On the ground in Uganda
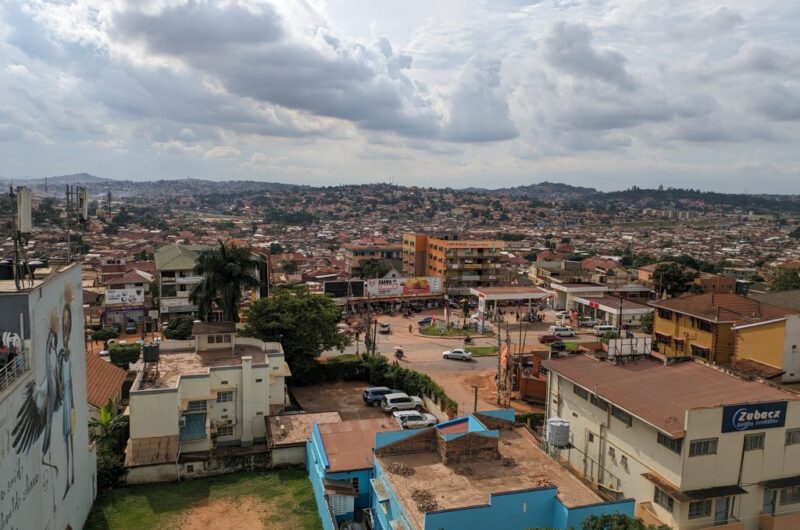
On 4 June I finally arrived in Entebbe after a long overnight flight with no sleep. I didn’t feel tired though, I was too excited to see what wonders Uganda would offer. We met our driver soon after arrival and were in the van in no time. Even though we took the longer route back to the hotel, I really enjoyed seeing the scenery and we even drove past the Zika Forest! It was nice to get to the hotel though and relax for a few hours, including enjoying the view from the hotel rooftop bar.
The next few days were very busy – on Monday I co-chaired two stakeholder engagement workshops with representatives from MoH, NDA, IDI, patient representative groups, etc. It was important to inform them of the upcoming study and get their thoughts on the issue of AMR in the country. The team at the Academy for Health Innovation at IDI had worked so hard to prepare for the workshops and, because of this, the workshops went off without a hitch. I also attended meetings with the data collection team and in-country members of our project team to discuss data collection and understand local customs that may impact the data collection, including the need for a member of the local government to chaperone us while we were conducting the surveys.
Finally, the big day arrived on Thursday. Data collection day! Early that morning we all piled into a van that took us to an area within Kawempe Division, Kampala where we got out and dispersed to go to different dispensaries. Even though it was the first day, I was really struck by the high participation rate. Almost everyone we approached was happy to take part in the study. It was also really nice to get out from behind a desk and physically seek out participants for the study, harkening back to the days when “shoe-leather” epidemiology was frequently practiced.
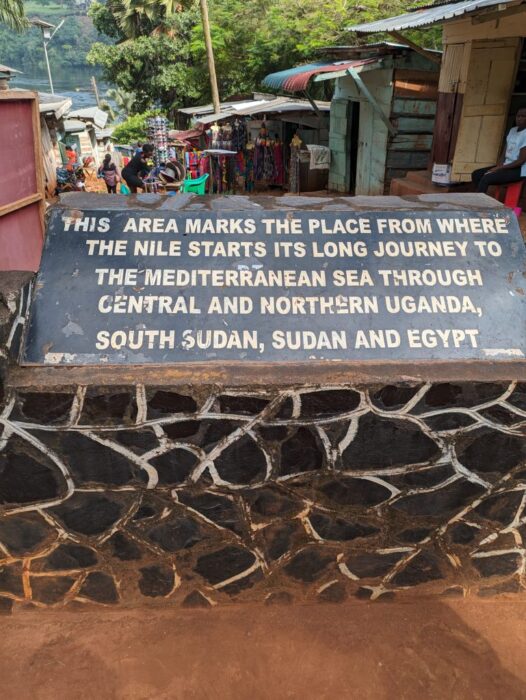
After our busy first day of data collection, it was a surprise to hear that Friday was a national holiday in Uganda and all offices would be closed. I therefore decided to escape the city for a while and take a day trip to the countryside. On the advice of the team, I went to Jinja in the early morning to see the source of the Nile (being related to David Livingstone, this was really exciting for me). During the trip, I was really shocked to hear about the impact of climate change and see the results first hand. My driver took the boat trip with me and discussed how he used to come here when he was younger. At that time, there was a café in the centre of the river but now the water level has risen so high that it is completely flooded.
On the trip, I also sampled the local cuisine at a small café, took a long walk in Mabira Forest, and was involved in a small car accident on the drive back to the hotel. The person who hit us kept driving, and this resulted in my driver pulling over to the side of the road, telling me he would come back for me, and then jumping on to a boda boda to speed off after them. Sitting in a car at the side of the road somewhere between Jinja and Kampala in the late afternoon, I started to question my life choices but had faith all would be well. He did, of course, eventually come back and the rest of the trip to the hotel was thankfully uneventful.
The final week went by really quickly and was a mix of data collection and interviews. I was amazed that we actually completed all of our data collection during that time. The IDI team worked so hard and this project would not have been possible without them.

Project findings
While the final report is yet to be completed, some initial findings from the study are worth considering. These findings are consistent with similar studies conducted in other countries and can help to inform action going forward.
- In general, dispensers have appropriate knowledge of AMR and AMS
- Dispensers agree that AMS should be practiced within community dispensary settings
- Actual practices related to AMS are variable
- It is not clear how information on resistance gets back to dispensers in the community
So here I am, at the end of my Fellowship. The final report will be done soon and then shared with stakeholders in order to get their views and decide next steps. It has been a very busy year, but exciting times are ahead and I look forward to continuing to support the partnership in the coming months.
Return to blogs