By Barida Poi
In this blog, Global Health Fellow Barida Poi discusses her experience with the Kakamega Cambridge Antimicrobial Stewardship Partnership, helping to deliver training in infection control, management of sepsis and postnatal care in a maternity setting.
Barida Poi is an Obstetrics and Gynaecology specialist trainee with a keen interest in global health and a passion for education and improving outcomes in women’s health. She is a 2023 East of England Global Health Fellow and here she describes her experience working within the Kakamega Cambridge Health Partnership. In particular she describes a visit to Kakamega County Teaching and Referral Hospital in Western Kenya, to co-deliver training in management of sepsis and infection control in a maternity setting.

Background
In 2015, all member states of the United Nations pledged to achieve peace and prosperity for the planet and its inhabitants, from that moment and for generations to come. This led to the genesis of the Sustainable Development Goals (SDGs), a set of 17 goals aiming to be achieved by 2030[1].
As an East of England Global Health Fellow and an Obstetrics and Gynaecology Registrar, one goal that resonates with me is SDG Target 3.1: To reduce the global maternal mortality ratio (MMR) to less than 70 per 100,000[2].
In the UK we have achieved this with a ratio of 6 per 100,00 between 2018-2020[3], however in Kenya, this value is much higher at 355 per 100,000[4].
The partnership project
The Kakamega Cambridge Antimicrobial Stewardship partnership (funded by the Commonwealth Partnerships for AMS) between Kakamega County Teaching and Referral Hospital (KCTRH), Masinde Muliro University of Science and Technology (MMUST), Cambridge University Hospitals NHS Foundation Trust and CGHP, laid the foundation to reduce the maternal mortality ratio by tackling the issue of Antimicrobial Resistance and Stewardship. As part of this, a team from Kakamega visited Cambridge University Hospitals (CUH) in May 2022 and highlighted sepsis as a major cause for concern and a major contributing factor to the maternal mortality rate in their maternity unit. While the issue of lowering the MMR is complex and multifaceted, sepsis is avoidable, and when identified in a timely manner, is reversible to a full recovery.

As part of my Global Health Fellowship and following extensive planning, I had the opportunity to visit Kakamega with three others from East of England and collaborate with the team, to co-create and co-deliver a training course addressing Assessment and Management of Sepsis Infection Prevention Control, and Postnatal care to 77 delegates over three days. Through this course, we were able to introduce the use of simulation training and the utilisation of the Modified Obstetric Early Warning Score (MEOWS) to reinforce and simplify the identification of at-risk patients who required urgent review and treatment.
We were assisted in this process by Mercy Adera, a staff nurse at CUH, who grew up near Kakamega and was able to provide pertinent insight into working both in Kenya and the UK, and how best to amalgamate her experiences with the intention of the course.
The course was well received, with high levels of engagement and positive feedback. However, several questions arose in the process:
- How can the knowledge and insight be sustained long term?
- What can we do to ensure the lessons learned are not forgotten once the novelty of the training and the visits fades?
- How can the learning from this course benefit the wider community outside of the Level 5 hospital?
- What resources are needed to minimise the delay in identification of sepsis and commencement of management?

Taking on board the feedback received, and after assessing the capacity of the maternity team, there was budget available to refurbish the education room in the hospital to make it suitable for simulation training, and to continue to deliver the training to more and other staff, utilising the learning materials from the course.
Alongside this, we were able to allocate and train ‘Sepsis Champions’ in the form of representatives from Level 4 hospitals across Kakamega County, to disseminate the knowledge gained from these sessions. We also produced and distributed educational posters and small business cards with the important takeaway messages from the training. Finally, to shorten the delay between identification and treatment, we were able to create sepsis boxes. These included essential equipment needed to begin bedside investigations, with copies of the MEOWS charts and protocols for the commencement of antibiotics. These were distributed across hospitals with staff who attended the training. The sepsis boxes were placed in the maternity units at Kakamega County Hospital and at three Level 4 hospitals in Kakamega county.

Reflections
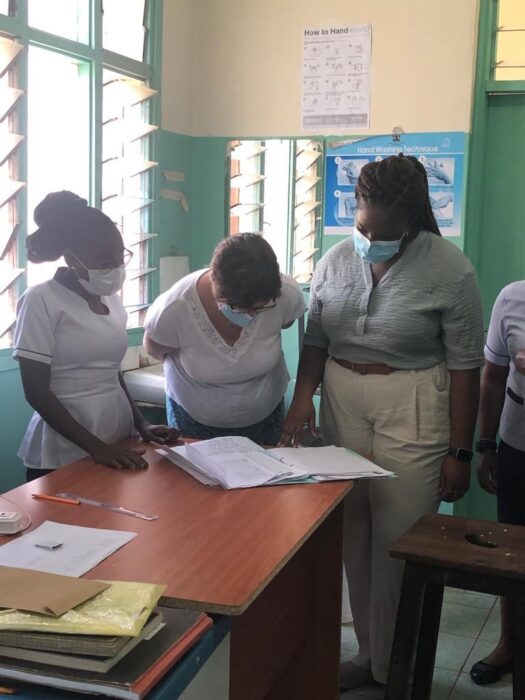
It was extremely fulfilling to see positive changes in the department and the healthcare professionals in such a short period of time. As part of the course, we conducted ward rounds in the clinical areas to highlight areas of improvement from an Infection Prevention and Control perspective. By day three, changes were already evident in the labour ward and antenatal wards.
This project was an incredible opportunity to meet the team face-to-face. It allowed me to hear first-hand the issues and challenges they face in the provision of safe care for the women and infants on the unit; as well as supporting them in improving the services and care. Maternity care has many challenges worldwide. However, the maternity team at KCTRH worked together seamlessly and resiliently in spite of the limited resources available to deliver exceptional care to their patients. This visit demonstrated the beauty of health partnerships in reciprocal learning.
While we were there to support the delivery of the course, I was able to learn about the healthcare systems in Kenya; further develop my problem-solving skills by facing the challenges that arose along the way; conduct case-based discussions from previous complex cases faced by the clinicians; and better understand the importance of technology in facilitating multidisciplinary teaching in a post-Covid healthcare setting.
Future developments
Going forward, the goal is to:
- Co-develop sepsis management guidelines and implement regular simulation training. Co-create relevant health messages videos for women and display them in the post-natal wards in local languages.
- audit improvements in hand hygiene practices building on the creation and display of sepsis and hand hygiene posters on the wards.
References:
1. Explained: The Sustainable Development Goals. Available at https://sdgs.un.org/goals/goal3 Last accessed 14/5/2023
2. SDG Target 3.1 Maternal mortality. Available at https://www.who.int/data/gho/data/themes/topics/sdg-target-3-1-maternal-mortality#:~:text=SDG%20Target%203.1%20Reduce%20the,manage%20complications%20are%20well%20known Last accessed 14/5/2023
3. Maternal mortality rate per 100,000 maternities, and maternal mortality ratio. Available at https://sdgdata.gov.uk/3-1-1/ Last accessed 14/5/2023
4. Maternal Health in Kenya. Available at https://kenya.unfpa.org/en/topics/maternal-health-16 Last accessed 14/5/2023
Find out more about how you can apply for the Global Health Fellowship Scheme or email info@cghp.org.uk.
If you are interested in supporting CGHP, please follow the donate button below or contact the team.
Return to blogs

