A team of Cambridge University Hospitals NHS Foundation Trust (CUH) paediatric haematology and oncology staff spent last week in Kampala, working alongside their counterparts at the Uganda Cancer Institute.
Consultant Paediatric Haematologist Dr Emmy Dickens, Research Nurse Amanda Semerene and Non-Malignant Haematology Clinical Support Nurse Joanne Neville are part of the CGHP-supported Paediatric Cancer Partnership which aims to improve outcomes for children with cancer – both in Uganda and the UK.
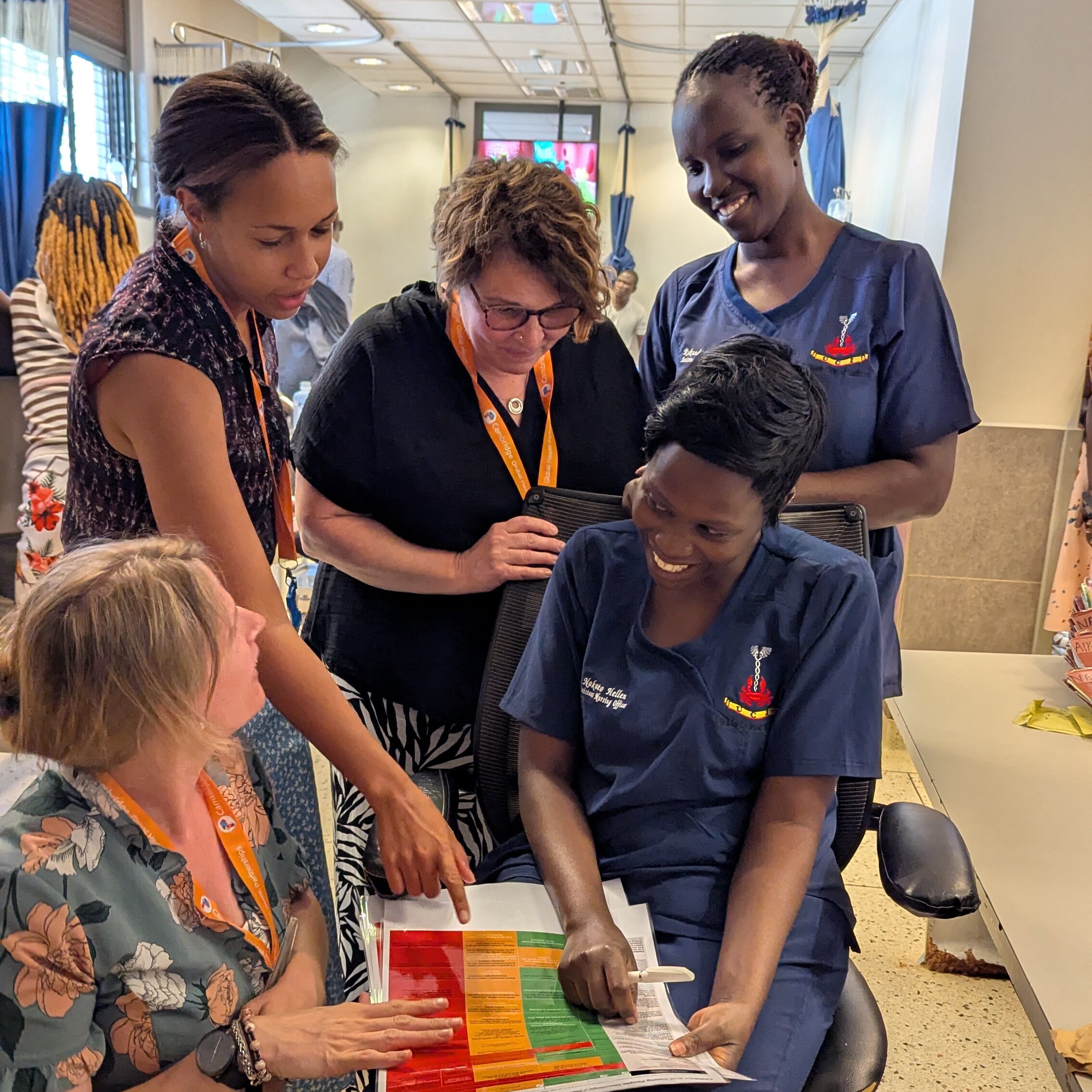

The team were joined on the visit by CGHP East of England Global Health Fellow and Paediatrics trainee Anna Muwanga. Anna has been working alongside the nurses from both sites on a Paediatric Oncology Triage Tool, based on the triage toolkit from The Children and Young People’s Cancer Association (CCLG) and already audited on 80 patients at UCI. The visit was an opportunity to refine the tool at UCI and make improvements to the process so it’s ready to embed as standard practice in the Paediatric Outpatient Department (OPD) at UCI. Further development plans include bringing together the early warning score in use on the ward and parent/caregiver education on signs of deterioration. Knowledge exchange is a key component of health partnerships and being able to collaborate and share learning like this helps develop protocols and practices most effective for the local context.
After a year of working together virtually, the visit was a valuable opportunity to build deeper relationships that are such an important part of longstanding health partnerships. The nurses had not met in person before and this face-to-face, onsite connection was necessary to understand the resources and skills available at UCI to underpin development of policies and standard operating procedures for patient care, at the request of the UCI paediatric lead nurses Susan Nabakooza and Mariam Ndagire.


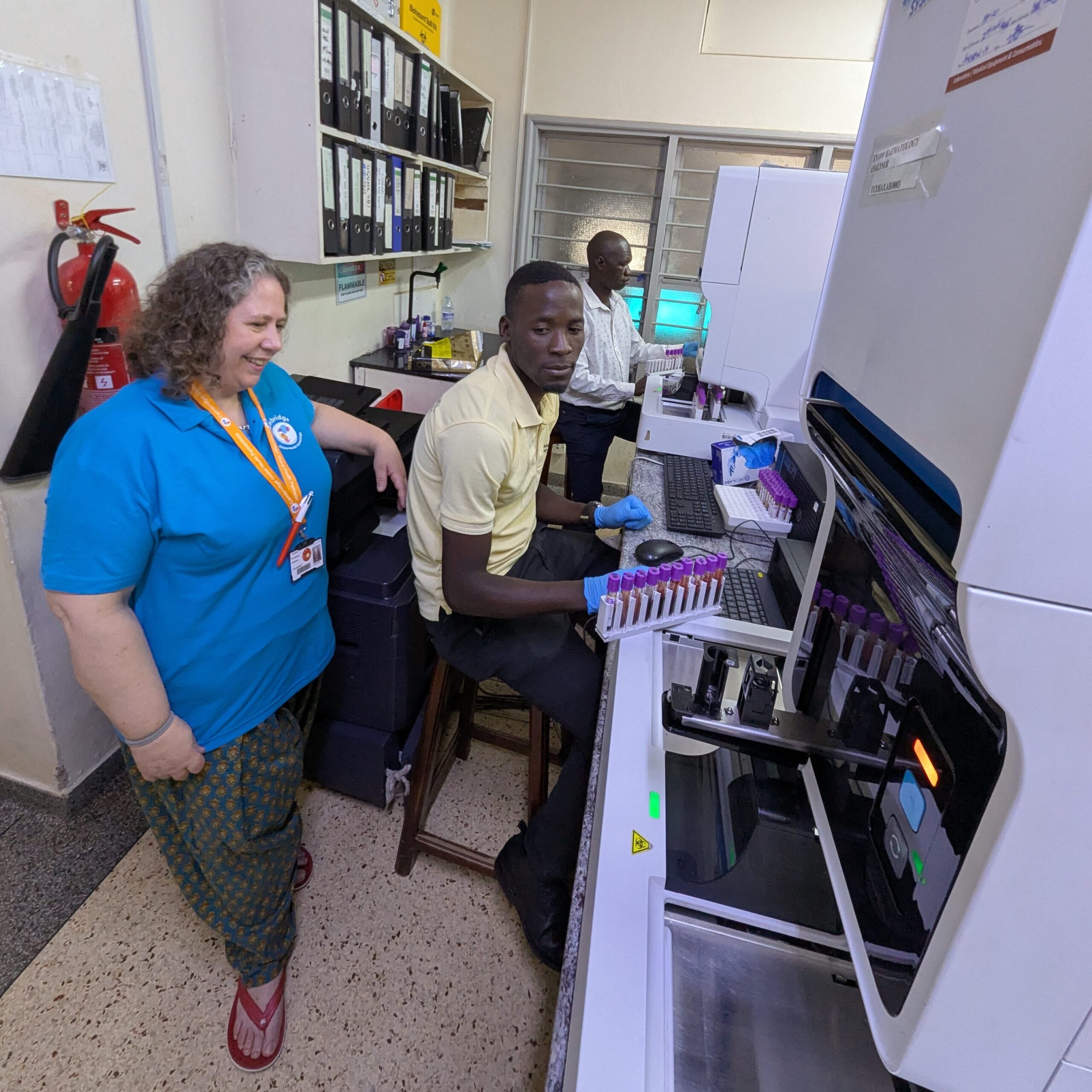
Emmy and the team were able to follow the chemotherapy process from the patient arriving and being reviewed, prescribing, communication with pharmacy, making up the drugs, delivery to the unit and ultimately administration to the child. A similar review of the transfusion process was also followed, including observing “white tile” forward blood grouping processes in the laboratory.

Other notable highlights included attending tumour board meetings to discuss complex patients; following patients through the outpatient process and to the chemotherapy administration area; attending a sickle cell disorder outpatient clinic; speaking to nurses, doctors, allied health professionals and families on the ward and visiting the Uganda Child Cancer Foundation. All this will underpin the ongoing partnership work to develop safety and quality processes to ensure that more children receive timely and relevant chemotherapy.


Find out more about the Paediatric Cancer Partnership and support the work here.
Return to news

