Annalan Navaratnam is a Public Health Registrar and East of England Global Health Fellow involved in CGHP’s long-standing health partnership with Myanmar. Here he reflects on the incredibly difficult circumstances our Myanmar partners are operating in and the many learnings to be taken from their wide-reaching telemedicine service that is providing a lifeline for conflict – and now earthquake – affected communities.
“Think back to 1 February 2021. What were you doing? What were your aims for the year?
We’d just been through a devastating year of a global pandemic that brought the world to its knees. It was a time where global alignment of country priorities had never been so important. Everyone was trying to build back.
In the UK, the headlines of that date focused on how to roll out COVID-19 vaccines as quickly as possible, rebuild our healthcare system and identify those who had been left behind to repair the direct and indirect damage of a global pandemic. This was the case across the globe, including in Myanmar where the democratically elected government were about to roll out a national COVID-19 surveillance system.
On 1 February 2021, this and many other initiatives to help the people of Myanmar were disrupted by the military coup d’etat who overthrew the democratically elected government, undoing a decade of progress. Under the military regime, violence against civilians escalated, with thousands jailed, tortured, or killed. In 2024, the UK government estimated that 2.6 million people had been displaced from their homes.
There were 411 incidents against healthcare systems within the first year of the military regime, 535 arrests of health workers, 118 raids and occupations of health facilities, and 29 health workers killed. And this pattern continued year upon year.
What emerged from these atrocities was a unification of healthcare professionals to develop other ways to provide access to healthcare while maintaining security for the patients and providers.
Delivering healthcare in the most challenging conditions
In June 2021, thanks to the dedication of healthcare workers from Myanmar and with support from Cambridge Global Health Partnerships, a free online telemedicine service was established. It provides quality healthcare and support to people of Myanmar, focusing on conflict-affected populations and internally displaced individuals. The vision isn’t just about providing care but building capacity to create sustainable and integrated services, and the remit of the telemedicine service has expanded beyond the COVID-19 response.
To date there are 303 providers running 13 primary care and 23 specialist clinics for over 72,000 patients, totalling over 200,000 tele-consultations. This is all from healthcare professionals volunteering their time and putting themselves at risk to help those most in need.
The telemedicine charity delivering these services faces increasing challenges with funding, maintaining the safety and security of providers and patients, and overcoming disruption to infrastructures – for example because of electricity being cut off, social media being banned, or VPNs being blocked.
Despite this, with CGHP’s support, they remain ambitious and want to establish training and education programmes, quality assurance processes, and build their research capacity. It’s this ambition that aligned with my reasons for applying for the East of England Global Health Fellowship – to better understand ways to strengthen health systems and be an innovative public health leader.


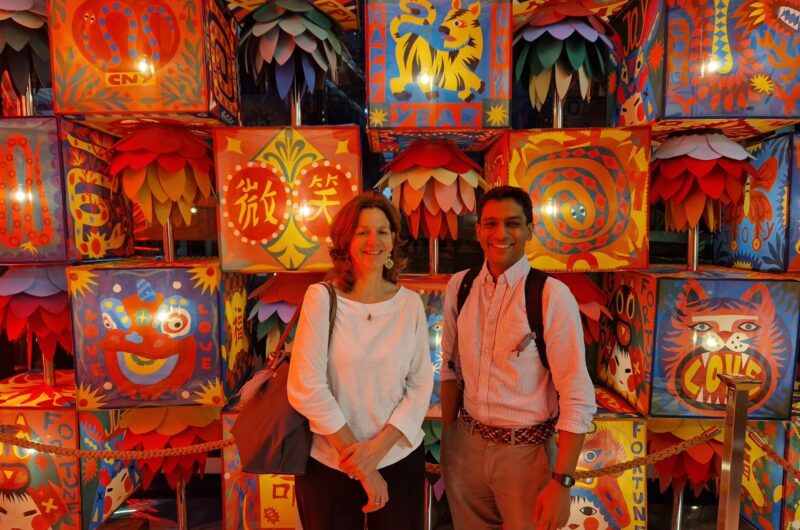
Left: CGHP Director Evelyn Brealey with Annalan. Right: Annalan presenting QA workshop to Myanmar partners.
Meeting face to face for the first time
In February, the CGHP team and I visited Bangkok to meet safely with Myanmar partners, including the charity’s senior leadership team. We compressed years’ worth of work into three days of meetings to review programmes and funding, monitoring and evaluation, and support the development of their quality assurance (QA) strategy and activities. QA processes were created by reviewing an array of UK and international frameworks, for both clinical and telemedicine care to produce a ‘menu’ of domains. Together we decided on three QA priorities: patient satisfaction, staff satisfaction and motivation, and clinical effectiveness. For each of these areas we reviewed anecdotal evidence to form ideas on potential activities and discuss risk of actions and inaction. These discussions didn’t just benefit the Myanmar team; they provided vast insights into novel approaches to tackle three priorities that affect the UK’s health systems.
Learnings and reflections
I have learnt many things that can be applied in my practice as a public health doctor. I gained insight into innovative approaches to increase accessibility in hard-to-reach areas. I formed ideas on how we can better utilise telemedicine in healthcare services and health improvement campaigns, coupled with social media to strengthen key messages. I observed ideas on how to create integrated multi-speciality models of care through tele-touring, a process where patients have a one-stop clinic in their own home. I learnt ways to unite and motivate health workforces and appreciated how international collaborations can inspire.
I’d like to thank the team at Cambridge Global Health Partnerships and the Myanmar partners for an inspiring experience. I am very fortunate to have the opportunity to contribute to strengthening a partnership across continents. A partnership that aims to support those most in need and fight injustice.”
To support our Myanmar partners in their response to the devastating earthquake and allow them to expand their vital service to those most in need, please donate to CGHP’s Emergency Appeal.
Applications for the 2026 East of England Global Health Fellowship open in the Spring.
Return to blogs